Introduction
Seventh-day Adventists have known about the benefits of healthy plant-based nutrition, exercise, self-control, adequate sleep, abstinence from alcohol, and many other lifestyle principles, for over one hundred years. However, despite the known benefits of these lifestyle practices to human health and flourishing, many Adventists are still timid, unenthusiastic or down-right opposed to sharing these principles. In this article, I argue, within the context of the COVID-19 and obesity pandemics, why the world desperately needs the Adventist health message.
Obesity, a Major Comorbidity
For the past several months, we have been witnesses to a colossal collision of two great pandemics: the obesity and COVID-19 pandemics.1 We know this because a bountiful number of studies have clearly established that a relationship between excess adiposity (body fat) and more severe COVID-19 exists.2,3 For example, obese COVID-19 patients:
make up the majority of hospitalized COVID-19 patients.4 One study in New York reported that 61% of the 4000 + COVID-19 patients were obese.5
may have up to a threefold greater risk of advancing to a severe or critical state.6
are more likely to require intensive care.7,8
are more likely to require mechanical ventilation.9 A study out of Lyon, France found that 81% of obese patients needed ventilation compared to 41% of lean patients.10
will likely stay at the hospital for longer than lean patients (23 days vs 18 days).6
have a higher risk of death from COVID-19.4,11. One study of over five thousand patients suggests that the risk is doubled.12
The location of the fat seems to be important as well. Studies from Germany and Rome both found that more fat around the abdominal organs (visceral fat) is associated with a greater need for intensive care and mechanical ventilation.13,14
This obesity-Covid link is so strong that the European Association for the Study of Obesity released a position statement stating:
“It may seem counterintuitive that COVID-19, a communicable disease, has such contiguity with non-communicable diseases such as obesity. However, people with obesity have an elevated risk of hospitalization, serious illness, and mortality, likely due to chronic low-grade inflammation, and altered immune response to infection, as well as related cardio-metabolic comorbidities, and the COVID-19 pandemic is likely to have a significant impact on people with obesity.”15
Why Might Obesity Worsen COVID-19?
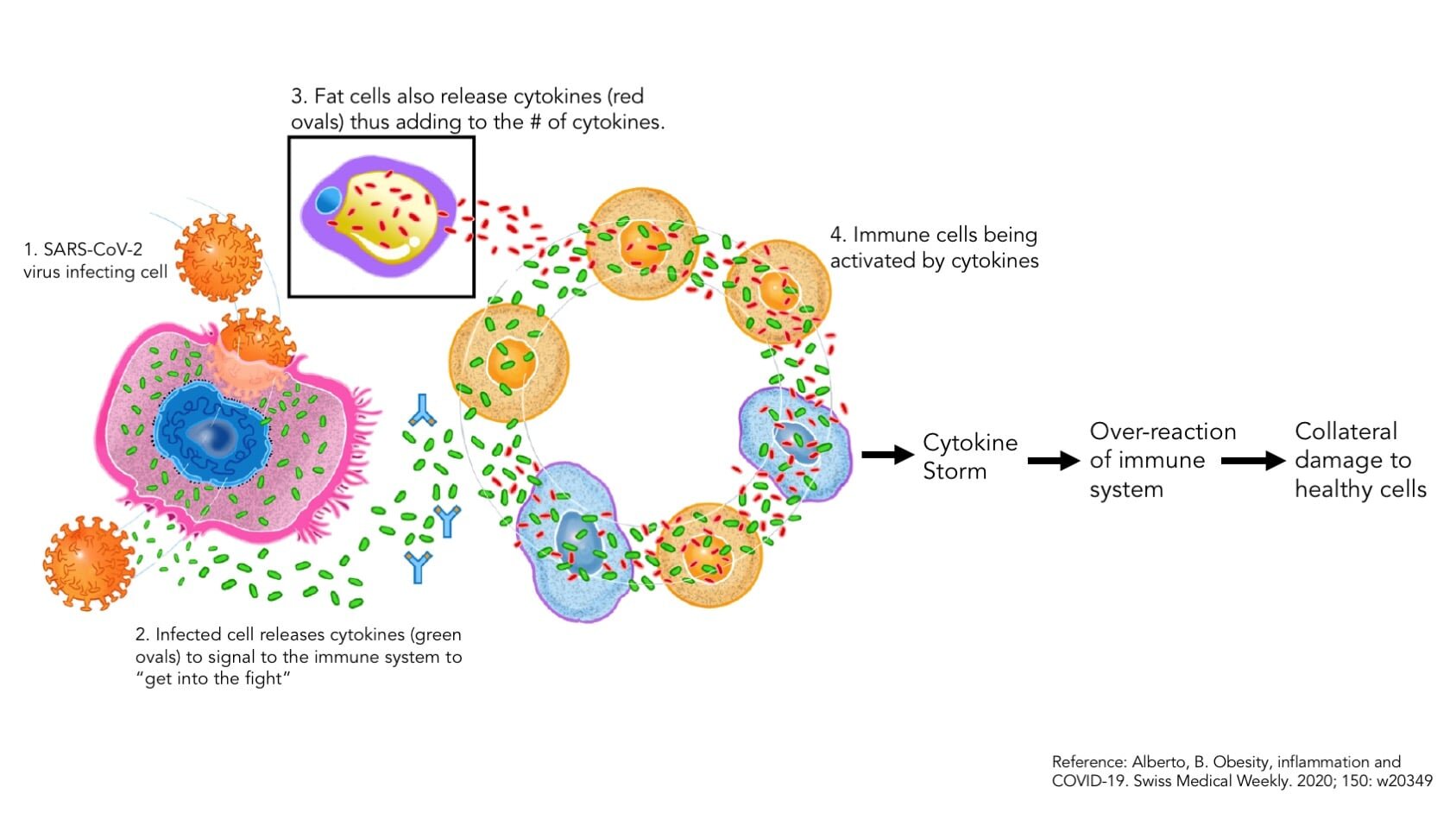
Why does obesity result in a more severe presentation of COVID-19? To answer this, people have to understand Cytokine storm. In many cases, cytokine storm is the physiological process that likely drives the body towards severe COVID-19.2,16 Cytokines are protein messengers that, to put it simply, activate the immune system to “get into the fight.” As the name suggests, cytokine storm is when there are a lot of cytokines being stimulated.2 This might seem to be a good thing at first, since more cytokines (messengers) means more immune cells and more immune cells means more soldiers to fight off the pathogen. However, too much is detrimental because a “hyper activated” immune system will cause collateral damage to healthy cells.17 It is like a war. During war, not only do enemies die, but innocent people die as well. Similarly, during cytokine storm, a massive number of immune cells will be mobilized, and in the ensuing battle, the surrounding lung tissue will get damaged. As a result, fluid starts building up, and the lungs become stiffer (fibrosis).3 All this makes it difficult to breathe.
The Obesity – Cytokine Storm link
How does obesity contribute to cytokine storm? Obesity presents with several features that make cytokine storm more likely to occur. The main one is that obesity puts the body in a pro-inflammatory state.18 “Pro-inflammatory” means promoting inflammation. Generally speaking, obese individuals have a higher level of inflammation compared to leaner people. Fat cells (adipocytes) are crucial endocrine organs, necessary for the proper functioning of the human system. However, in the obese state (excess fat), the adipose tissue changes composition, structure, and function and become very pro-inflammatory.3,19 Thus, when an obese individual gets infected with SARS-CoV-2, the number of cytokines already being released from fat cells plus the cytokines now being released by infected lung cells, results in massive cytokine and immune cell activation; ie. cytokine storm.20 Then, as SARS-CoV-2 multiplies, it is easy to see how this can result in a dysregulated immune response. It is like adding fuel to the fire. Obesity is the pre-existing fire, and the SARS CoV-2 virus is like the fuel.
Obesity also has other features that may lead to severe COVID-19. For example, ACE2 is the main receptor used by SARS CoV-2 to invade cells. Adipose cells (adipocytes) express the ACE2 receptor.21 In fact, in obesity, the number of ACE2 receptors are upregulated.3,21 This means an obese individual may have more of the receptors available for SARS-CoV-2 infection. Obesity also reduces the cell killing ability (cytotoxicity) of Natural Killer cells; a potent immune cell.18 On top of this, hypertension, diabetes and heart disease are major comorbidities that are believed to exacerbate COVID-19. Obesity is linked with each one of these diseases.3
Similar Patterns Found with Prior Viral Infections
The obesity-virus link is not a new one. Previous infections have demonstrated that obesity worsens the prognosis of viral infections. For example, consider this short passage from an article published in the journal, Acta Diabetologica:
“Since the “Spanish” influenza pandemic of 1918, it is known that malnutrition (both under - and over-nutrition) is linked to a worse prognosis of the viral infection. The 1957 – 1960 “Asian” and the 1968 “Hong Kong” influenzas confirmed that obesity and diabetes lead to a higher mortality as well as a more prolonged duration of illness even if the subjects were without other chronic conditions…. During the 2009 Influenza A virus H1N1 pandemic, obesity was also linked to increased risk of severe disease and a risk factor for hospitalization and death.”22
This shows that the obesity-COVID link is not a novel association. Obesity has been linked with worse outcomes for other viral infections.
When we Adventists read information like this, it ought to stir our souls to the inner core because we are stewards of a precious health message that can help protect and even save lives in situations like the COVID-19 pandemic.
People Need our Health Message
Estimates from the World Health Organization suggest that obesity has tripled since 1974, and currently almost 2 billion adults are overweight. 650 Million of these are obese.23 Obesity will continue increasing thus putting greater proportions of the world population at increased risk for this and future pandemics. These should not be mere statistics to us. These individuals are our neighbors, friends, and family. These are God’s creation.
However, the good news is that there is an answer. Adventist health principles such as whole-foods plant-based nutrition, eating in a self-controlled manner, having two meals per day with a lighter third meal (if necessary), no eating between meals, abstinence from alcohol, physical activity, adequate sleep, and self-control, all can be very helpful.
In our practice, the majority of patients are assisted with weight management. I can testify with conviction that Adventist health principles do work. Weight loss and lasting results are possible, but the important thing is for people to be approached with compassion and tenderness. Also, I have found that people will take you seriously if they sense conviction from you. When it comes to the health message and weight loss, I project conviction to patients because Adventist health principles are backed up by scientific evidence and grounded in divine revelation. We have nothing to be ashamed of or timid about when it comes to our health message.
Do you have loved ones who are struggling with their weight? With hearts full of the sympathy and compassion of Jesus, pray for an opening to reach out to them. When that opening comes, tenderly, respectfully yet with firm conviction, share these principles with them. Show them unconditional respect. Encourage them when they falter, and balance them when they are in danger of going too extreme. Be a patient listening ear to their struggles and an enthusiastic cheer-leader with their successes, even if they seem small. People on a weight loss journey need all the encouragement they can get (remember most have probably been put down by friends and family, and have likely tried many failed diets). Many individuals are desperate to get to a healthy weight and we Adventists have a treasure-trove of knowledge that can be potentially powerful and life-changing.
Conclusion
Some are predicting that the COVID-19 lockdowns and the subsequent financial and social impacts may worsen the already-existent obesity crisis.24-26 It is also a certainty that though this current pandemic will pass, future pandemics will arise, likely manifesting a similar association with chronic diseases like obesity. In light of this, does it not behoove us as Adventists, possessing so much light on health, to live and share the health message as enthusiastically as we can to our fellow brothers, sisters, family, friends and neighbors?
Dr. Cho is a licensed naturopathic doctor who practices in Toronto, Canada.
References
1. Honce R et al. A tale of two pandemics: Obesity and COVID-19. J Travel Med. 2020 Aug 20; 27 (5): taaa097
2. Katzmarzyk, P., Salbaum, JM & Heymsfield, S. Obesity, noncommunicable diseases, and COVID-19: a perfect storm. Am J Hum Biol. 2020 Aug 14; e23484. Doi: 10.1002/ajhb.23484
3. Ritter, A et al. Obesity and COVID-19: Molecular mechanisms linking both pandemics. Int J Mol Sci. 2020, 21, 5793; doi:10.3390/ijms21165793
4. Ejaz, H et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infection & Public Health (2020).
5. Richardson, S et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area JAMA. 2020 May 26; 323 (20): 2052 – 2059
6. Gao, F et al. Obesity is a risk factor for greater COVID-19 severity. Diabetes Care. 2020 May ; dc200682
7. Petrilli, C et al. Factors associated with hospitalization and critical illness among 4103 patients with Covid-19 disease in New York city. medRxic. (2020)
8. Barrasa, H. et al. SARS-CoV-2 in Spanish Intensive Care: Early experience with 15-day survival in Vitoria. Anaesthesia Critical Care and Pain Medicine (2020), doi: https://doi.org/10.1016/j.accpm.2020.04.001
9. Simonnet, A et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. (2020). Doi: 10.1002/oby.22831
10. Caussey, C et al. Obesity is associated with severe forms of COVID-19. Obesity. 2020 Apr 21. doi: 1002/oby.22842
11. Zheng, Z et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J infect. 2020 Apr 23; S0163 – 4453 (20) 30234-6
12. Czernichow, S et al. Obesity doubles mortality in patients. Hospitalized for SARS-CoV-2 in Paris hospitals, France: a cohort study on 5795 patients. Obesity 2020 Aug 20. Doi: 10.1002/oby.23014
13. Petersen, A et al. The role of visceral adiposity in the severity of COVID-19: Highlights from a unicenter cross-sectional pilot study in Germany. Metabolism Clinical and Experimental 110 (2020) 154317
14. M. Watanabe, D. Caruso, D. Tuccinardi, et al. Visceral fat shows the strongest association with the need of intensive care in patients with COVID-19, Metabolism (2020), https://doi.org/10.1016/j.metabol.2020.154319
15. Fruhbeck, G et al. European Association for the Study of Obesity Position Statement on the Global COVID-19 Pandemic. Eur J Obes. 2020
16. Tay, M et al. The trinity of COVID-19: immunity, inflammation and intervention. Nature Reviews Immunology. 2020
17. Alberto, B. Obesity, inflammation and COVID-19. Swiss Medical Weekly. 2020; 150: w20349
18. Caci, G et al. COVID-19 and obesity: Dangerous liaisons. J Clin Med. 2020, 9, 2511
19. Wensveen, F & Valentic, S et al. The “Big Bang” in obese fat: Events initiating obesity-induced adipose tissue inflammation. Eur J. Immunol. 2015. 45: 2446 – 2456
20. Ryan, P & Caplice, N. Is adipose tissue a reservoir for viral spread, immune activation and cytokine amplification in Covid-19. Obesity. 2020 Apr 21. Doi: 10.1002/oby.22843
21. Al-Benna, S. Association of high level gene expression of ACE2 in adipose tissue with mortality of COVID-19 infection in obese patients. Obesity Medicine 19 (2020) 100283
22. Luzi, L & Radaelli, M. Influenza and obesity: its odd relationships and the lessons for COVID-19 pandemic. Acta Diabetologica (2020) 57: 759 – 764
23. World Health Organization obesity facts: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
24. Clemmensen, C et al. Will the COVID-19 pandemic worsen the obesity epidemic? Nat Rev Endocrinol. 2020 Sep; 16 (9): 469 – 470
25. Khan, ABM & Smith, J. “Covibesity,” a new pandemic. Obesity Medicine 19 (2020) 100282
26. Bhutani, S & Cooper, J. COVID-19-related home confinement in adults: weight gain risks and opportunities. Obesity 2020